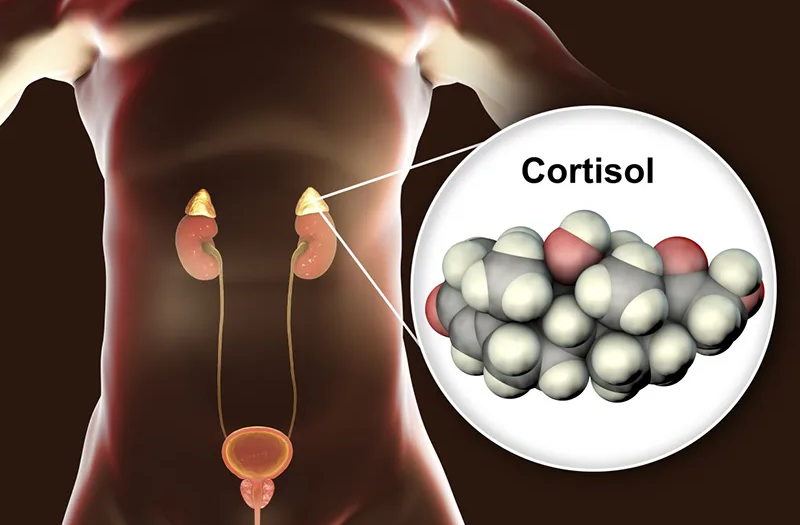
Cortisol, a vital steroid hormone, emanates from the adrenal glands positioned atop each kidney. Its secretion escalates during periods of stress, coursing through the bloodstream. Maintaining an optimal cortisol equilibrium proves pivotal for overall health, as deviations—whether excess or deficiency—can precipitate various health complications.
Operating as a versatile agent, cortisol exerts its influence across multiple bodily systems. Among its crucial functions, cortisol aids in:
- Stress Response: Facilitating the body’s reaction to stressors or perceived threats, cortisol plays a pivotal role in mobilizing resources for coping mechanisms.
- Glucose Metabolism: Cortisol orchestrates the metabolism of glucose within the body, ensuring a steady energy supply during times of need.
- Blood Pressure Regulation: Through intricate mechanisms, cortisol helps modulate blood pressure levels, contributing to cardiovascular health and stability.
- Inflammation Control: Cortisol exhibits potent anti-inflammatory properties, playing a pivotal role in dampening immune responses and mitigating excessive inflammation.
Moreover, cortisol serves as a cornerstone of the ‘fight or flight’ response, an innate mechanism for navigating perceived dangers. The body tightly regulates cortisol production to maintain an optimal balance, ensuring its myriad functions proceed harmoniously.
What stimulates the adrenal glands to generate cortisol?
The secretion of cortisol from the adrenal glands is under the meticulous control of the pituitary gland. Nestled at the base of the brain, the pituitary gland, often dubbed the ‘master gland,’ exerts profound regulatory influence over various bodily functions.
Upon waking, engaging in physical activity, or encountering stressful situations, the pituitary gland springs into action. It dispatches signals prompting the adrenal glands to synthesize and release the requisite quantity of cortisol. This orchestrated interplay ensures the timely and tailored provision of cortisol in response to the body’s needs.
What are the repercussions of excessive or insufficient cortisol production?
Under normal circumstances, the body meticulously regulates cortisol levels to uphold optimal health. However, imbalances can occur, leading to either excessive or deficient cortisol production. Conditions such as Cushing’s syndrome result in hypercortisolism, characterized by an overabundance of cortisol, whereas Addison’s disease manifests as hypocortisolism, involving insufficient cortisol secretion.
Excessive cortisol production can manifest in various symptoms, including:
- Weight Gain: Particularly noticeable around the abdomen and face, excess cortisol can promote fat accumulation in these regions.
- Skin Changes: Thin and delicate skin, prone to slow healing and susceptibility to bruising, is a hallmark of excessive cortisol levels. Additionally, acne may occur, further indicating hormonal imbalance.
- Endocrine Effects: In women, hypercortisolism can lead to manifestations such as facial hair growth and irregular menstrual cycles, indicative of disrupted hormonal equilibrium.
Conversely, insufficient cortisol levels can precipitate a distinct set of symptoms, including:
- Chronic Fatigue: Persistent feelings of tiredness and lethargy are common manifestations of cortisol deficiency, affecting overall energy levels and vitality.
- Gastrointestinal Disturbances: Nausea and vomiting may ensue, reflecting the systemic impact of cortisol insufficiency on digestive function.
- Weight Loss: Unintended weight loss may occur due to metabolic dysregulation associated with cortisol deficiency.
- Muscle Weakness and Abdominal Pain: Reduced cortisol levels can lead to muscle weakness and abdominal discomfort, impairing physical function and quality of life.
Should any of these symptoms arise, a healthcare provider may recommend diagnostic measures, such as blood tests to assess cortisol levels, aiding in the identification and management of underlying hormonal imbalances.
Understanding Corticosteroid Medications
Corticosteroids, synthetic derivatives of cortisol, serve as crucial therapeutic agents in various medical scenarios. When endogenous cortisol production falls short, as observed in conditions like Addison’s disease, healthcare providers may prescribe corticosteroids to supplement deficient hormone levels.
Yet, the utility of corticosteroids extends far beyond hormone replacement therapy. Leveraging potent anti-inflammatory properties, these medications find application in the management of diverse ailments. Conditions characterized by inflammation, such as asthma, inflammatory bowel disease, and psoriasis, often benefit from corticosteroid intervention. Even in individuals with adequate endogenous cortisol production, corticosteroids may be prescribed to alleviate symptoms and mitigate inflammatory responses effectively.
However, it’s imperative to distinguish between corticosteroids and anabolic steroids. While the former serve therapeutic purposes under medical supervision, the latter—commonly abused for performance enhancement and muscle growth—pose significant health risks when used without appropriate oversight. Anabolic steroids diverge markedly from corticosteroids in their pharmacological properties and intended uses, emphasizing the importance of responsible medication management under professional guidance.
Exploring the Side Effects of Corticosteroid Therapy
Given their potent pharmacological profile, corticosteroids wield significant therapeutic potential but also harbor a spectrum of side effects, particularly with prolonged usage. Short-term administration typically carries minimal risk of adverse effects.
However, protracted courses of corticosteroid therapy may precipitate various side effects, including:
- Skin Thinning: Chronic corticosteroid use can lead to the thinning of the skin, making it more vulnerable to injury and bruising.
- Osteoporosis: Prolonged exposure to corticosteroids may accelerate bone loss, heightening the risk of osteoporosis and fractures.
- Metabolic Effects: Increased appetite and subsequent weight gain, especially concentrated around the face, are common manifestations. Moreover, corticosteroids can elevate blood sugar levels, potentially leading to diabetes.
- Mood Disturbances: Rapid fluctuations in mood, characterized by irritability, anxiety, or depression, may ensue with long-term corticosteroid use, and in severe cases, individuals may experience suicidal thoughts.
- Immunosuppression: Corticosteroids can suppress the immune system, raising the susceptibility to infections.
- Ocular Complications: Chronic corticosteroid use is associated with ocular conditions such as glaucoma and cataracts, necessitating regular monitoring of eye health.
- Hypertension: Elevated blood pressure may occur as a consequence of corticosteroid therapy, warranting diligent monitoring and management.
When prescribed corticosteroids, it’s crucial to engage in open dialogue with your healthcare provider regarding treatment duration, potential side effects, and strategies for monitoring and mitigating adverse reactions. Additionally, pharmacists can offer valuable insights into medication management and address any concerns or queries regarding corticosteroid therapy.