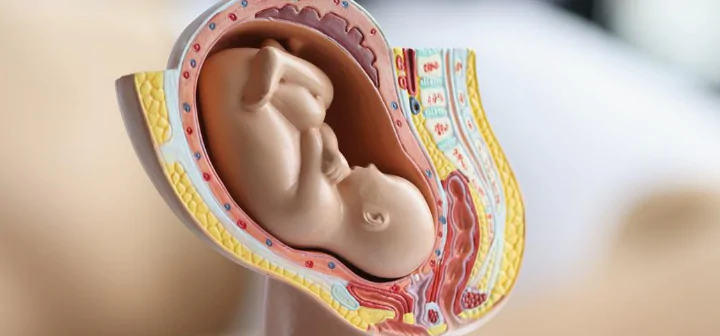
What you put in your body before becoming pregnant, during your pregnancy, and after the birth can have a significant impact on your baby’s health. Consuming a balanced diet rich in essential nutrients, avoiding harmful substances like alcohol and tobacco, and staying hydrated are crucial steps for a healthy pregnancy. Additionally, regular exercise tailored to your needs and seeking support from healthcare providers can enhance your overall well-being and contribute to a positive pregnancy outcome.
Smart Nutrition: A Guide to Healthy Eating for Optimal Well-Being
You don’t need to “eat for two” during pregnancy, but you do need to focus on quality nutrition. Your baby requires essential nutrients for healthy growth and development, so it’s crucial to increase nutrient-dense foods and reduce those high in salt, sugar, and unhealthy fats. Excessive intake of processed foods can lead to complications like gestational diabetes, high blood pressure, and unhealthy weight gain, affecting both you and your baby:
- nutrient-Rich Foods for Pregnancy. A balanced, varied diet is key to supporting a healthy pregnancy. It’s recommended to eat a wide range of fruits and vegetables of different types and colors daily, as they provide essential vitamins, minerals, and antioxidants. For example, leafy greens like spinach and kale offer folate, which is critical for your baby’s brain and spinal cord development, while citrus fruits provide vitamin C, boosting your immune system and aiding iron absorption.Whole grains are also a vital part of a pregnancy diet. Pregnant women should aim for 8 to 8 ½ servings of whole grains per day. Foods like oats, brown rice, and whole wheat bread supply energy, fiber, and important B vitamins that help reduce the risk of certain birth defects and promote healthy digestion;
- focus on Essential Nutrients. Iron is a crucial nutrient during pregnancy, as it supports the increased blood volume and helps prevent anemia. Iron-rich foods such as lean red meat, poultry, beans, lentils, and fortified cereals should be included in your daily diet. Pairing iron-rich foods with sources of vitamin C—such as tomatoes, oranges, or bell peppers—improves iron absorption. Calcium is another vital nutrient, supporting the development of your baby’s bones and teeth. Dairy products like low-fat milk, yogurt, and cheese are excellent sources of calcium, but if you prefer non-dairy options, fortified plant-based milks, tofu, and almonds can provide the calcium you need. Pregnant women should aim for about 1,000 mg of calcium daily. Protein is essential for fetal growth, particularly during the second and third trimesters. You can meet your protein needs by incorporating a variety of sources, such as lean meats, poultry, fish, eggs, tofu, beans, and legumes. Aim for 2-3 servings of protein-rich foods each day to support your baby’s growth and maintain your muscle mass;
- hydration and Constipation Relief. Drinking plenty of water is important for staying hydrated, maintaining healthy amniotic fluid levels, and supporting digestion. Pregnant women should aim for at least 8-10 glasses of water per day. Consuming fiber-rich foods like fruits, vegetables, and whole grains, along with adequate hydration, can help alleviate constipation, which is common during pregnancy;
- caffeine Guidelines. While it’s generally safe to have caffeine during pregnancy, it’s recommended to limit it to about 200 mg per day. This amounts to roughly 2 cups of coffee or 6 cups of tea. Too much caffeine can increase the risk of miscarriage or low birth weight, so monitoring your intake is essential. Remember that caffeine is also found in soft drinks, energy drinks, and certain medications, so check labels to stay within safe limits;
- food Safety Precautions. Pregnant women are more vulnerable to foodborne illnesses, so it’s important to take extra care with food safety. Avoid foods that carry a higher risk of contamination, such as raw or undercooked eggs, soft cheeses like brie or camembert, unpasteurized dairy products, pate, and deli meats. These foods can contain harmful bacteria like Listeria or Salmonella, which can lead to complications such as miscarriage or stillbirth. When preparing food, always practice good hygiene, such as washing hands and cooking surfaces thoroughly. Ensure that meats, poultry, and fish are fully cooked, and avoid cross-contamination between raw and cooked foods. Mercury in Fish. Fish can be an excellent source of omega-3 fatty acids, which are important for your baby’s brain and eye development. However, certain fish with high mercury levels—such as shark, swordfish, marlin, and tilefish—should be limited to one serving per fortnight. High mercury levels can negatively affect your baby’s developing nervous system. Safer options include salmon, sardines, and trout, which are lower in mercury and rich in omega-3s;
- supplements During Pregnancy. In addition to a healthy diet, certain supplements are recommended during pregnancy to ensure you meet your increased nutrient needs. Folic acid is vital for preventing neural tube defects and is recommended before conception and during early pregnancy. Iodine supports the baby’s brain development and prevents thyroid issues. Most women will benefit from a prenatal vitamin containing these key nutrients, along with other important vitamins like vitamin D and omega-3 fatty acids. Always consult your healthcare provider about the right supplements for you, as individual needs may vary.
By focusing on a nutrient-rich, balanced diet and following these guidelines, you can support your baby’s healthy development while maintaining your own well-being throughout pregnancy.
Incorporating smart nutrition into your daily routine is key to achieving optimal well-being. By focusing on a balanced, nutrient-dense diet and making mindful food choices, you can support long-term health, boost energy levels, and reduce the risk of chronic diseases. Remember, small, sustainable changes in your eating habits can make a lasting impact on your overall health.
Managing Healthy Weight Gain: A Balanced Approach for Pregnancy
Being overweight or obese during pregnancy is associated with a variety of health risks that can affect both you and your baby. These risks include complications such as stillbirth, preterm birth, birth defects, high blood pressure, gestational diabetes, and even postpartum depression. Being significantly overweight can also complicate the birth process, increasing the likelihood of requiring interventions like a cesarean section, and it may also affect your ability to breastfeed effectively. Overweight women will need extra monitoring and care throughout their pregnancy and childbirth to ensure both their well-being and that of their baby.
Conversely, being underweight during pregnancy also poses risks. Women who are underweight are at an increased risk of preterm labor and delivering a smaller baby, which can lead to health challenges for the newborn, including low birth weight and developmental delays:
- recommended Weight Gain During Pregnancy. Your healthcare provider will guide you on how much weight you should gain during pregnancy based on your pre-pregnancy body mass index (BMI). For women who begin their pregnancy at a normal weight, a healthy weight gain typically ranges between 11.5 to 16 kilograms (25 to 35 pounds). For overweight or underweight women, the recommended weight gain may be adjusted accordingly. Gaining too much or too little weight during pregnancy can lead to complications such as gestational diabetes, preeclampsia, or a small-for-gestational-age baby, so it’s important to follow your doctor’s advice and monitor your progress throughout the pregnancy;
- managing Weight During Pregnancy. If your doctor identifies that your weight gain is above or below the recommended level, they may refer you to a dietitian for personalized nutrition advice. A dietitian can help you create a balanced meal plan that supports healthy weight gain, focusing on nutrient-rich foods like fruits, vegetables, whole grains, lean proteins, and healthy fats. This approach will ensure that both you and your baby receive the essential nutrients needed for growth and development. It is important to note that strict dieting to lose weight during pregnancy is not advised. Restricting your calorie intake or following fad diets may deprive your baby of essential nutrients, leading to developmental issues and complications. Instead, the focus should be on balanced eating and maintaining a healthy lifestyle;
- exercise and Healthy Habits. In addition to a balanced diet, regular physical activity can help manage weight gain during pregnancy. Light to moderate exercise, such as walking, swimming, or prenatal yoga, can help maintain fitness, improve mood, and promote healthy weight gain. Always consult with your healthcare provider before starting any new exercise routine to ensure it’s safe for you and your pregnancy.
By working closely with your healthcare team and adopting a balanced approach to diet and exercise, you can achieve healthy weight gain during pregnancy and reduce the risk of complications for both you and your baby.
Alcohol and Pregnancy: Understanding the Risks and Making Safe Choices
Whenever you consume alcohol during pregnancy, it crosses the placenta and enters your baby’s bloodstream, directly impacting their development. Drinking alcohol increases the risk of serious complications, including miscarriage, stillbirth, and premature birth. The most severe consequence of heavy drinking is fetal alcohol spectrum disorders (FASD), which can cause long-term physical, behavioral, and cognitive problems. These issues can affect a child’s ability to learn, their social interactions, and their overall health throughout life.
If you had a small amount of alcohol before discovering your pregnancy, it’s unlikely to have caused harm. However, once you are aware you’re pregnant, it is crucial to avoid alcohol entirely. Research has shown there is no safe level of alcohol consumption during pregnancy. Even small amounts can increase risks, and the more you drink, the greater the potential harm to your baby. Binge drinking, defined as consuming large amounts of alcohol in a single session, is particularly dangerous and can severely affect your baby’s development, especially during the first trimester when major organs are forming.
Alcohol and the Baby’s Development. Drinking alcohol at any stage of pregnancy can interfere with your baby’s development. In early pregnancy, alcohol can affect the formation of the baby’s brain, heart, and other vital organs. Later in pregnancy, it can lead to growth restrictions and developmental delays. Children born with FASD may experience issues like poor memory, attention deficits, learning disabilities, and social difficulties. Some may also have distinct facial features or heart defects.
By avoiding alcohol and seeking support when needed, you can help ensure a healthier pregnancy and give your baby the best possible start in life.
Smoking and Pregnancy: Understanding the Risks and How to Quit for a Healthier Baby
Smoking and exposure to secondhand smoke during pregnancy pose serious risks to both you and your baby. Smoking increases the likelihood of pregnancy complications, such as preterm birth, miscarriage, and placental abruption. Additionally, it can lead to low birth weight, which is associated with a higher risk of health issues for your baby, including respiratory problems and developmental delays. Babies exposed to maternal smoking are also at a greater risk of sudden infant death syndrome (SIDS) and long-term health problems such as asthma and learning difficulties:
- quitting Smoking During Pregnancy. Many women successfully quit smoking when they learn they are pregnant, but relapses can occur. If you find yourself struggling to stay smoke-free, don’t be discouraged—it’s common and normal. Each attempt to quit is a step toward better health for you and your baby. Support from your partner can significantly increase your chances of quitting successfully, so encourage them to quit as well if they smoke;
- seeking Support. It’s crucial to be honest with your doctor about your smoking habits. Your healthcare provider can offer guidance and resources to help you quit, including nicotine replacement therapy (NRT) and counseling. NRT products, such as patches, gum, or lozenges, can help manage cravings and withdrawal symptoms, while counseling provides emotional support and strategies for overcoming addiction;
- resources for Quitting. Remember, it’s never too late to quit smoking during pregnancy. Quitting at any stage of pregnancy can benefit both you and your baby. Reach out to resources such as the Quitline for personalized support and additional information on quitting smoking. They offer free and confidential advice to help you through the process.
By quitting smoking and avoiding secondhand smoke, you are significantly improving your baby’s chances of a healthy start in life and reducing the risk of long-term health issues.
Quitting smoking during pregnancy is one of the most impactful steps you can take to ensure a healthier start for your baby and protect them from a range of serious health risks. With the right support and resources, you can overcome challenges and achieve a smoke-free pregnancy, significantly improving outcomes for both you and your baby.
Staying Active During Pregnancy: Benefits and Safe Exercise Guidelines
Pregnant women are encouraged to engage in some form of physical activity every day, gradually aiming for 150 to 300 minutes of moderate-intensity exercise each week. Staying active during pregnancy offers numerous benefits, including improved mood, better sleep, reduced back pain, and helping to prepare your body for labor.
Before starting or modifying your exercise routine, it’s important to consult your doctor about what activities are safe for you, especially if you have any pregnancy-related conditions. Low-impact activities like brisk walking, swimming, and stationary cycling are excellent options. Prenatal yoga and pilates can also help with flexibility, strength, and relaxation. Joining a group, like a walking club, swim group, or prenatal yoga class, can increase motivation and provide social support.
Be cautious to avoid activities that could put undue stress on your body, such as high-impact or contact sports that may injure your abdomen or strain your joints, as pregnancy can make your joints more vulnerable. Scuba diving is also unsafe for pregnant women due to the pressure changes, which can pose risks to the baby. It’s best to exercise during cooler parts of the day to avoid overheating and dehydration, and be sure to drink plenty of water before, during, and after physical activity to stay hydrated.
Immunization During Pregnancy: Protecting Yourself and Your Baby
Immunization during pregnancy is a crucial step in safeguarding both your health and your baby’s well-being. Vaccines like those for flu and whooping cough offer protection against serious infections that can pose risks to pregnant women and newborns. By staying up to date with recommended vaccinations, you help ensure a healthier start for your baby.
If you’re planning to become pregnant, it’s important to ensure you’re up to date on your rubella (German measles) and varicella (chickenpox) vaccinations. Contracting either of these infections during pregnancy can lead to serious complications, including congenital defects and developmental issues for your baby. These vaccines should be administered before pregnancy, as live vaccines are not recommended once you’re expecting.
During pregnancy, two vaccinations are strongly recommended to protect both you and your baby:
- influenza (Flu). Pregnancy increases your risk of serious complications from the flu, such as pneumonia, which can also be dangerous for newborns. The flu vaccine is the most effective way to prevent influenza and its complications. It is safe to receive at any stage of pregnancy and is provided free of charge to all pregnant women under the National Immunization Program (NIP);
- whooping Cough (Pertussis). Whooping cough is highly contagious and can be deadly for newborns who are too young to be vaccinated. To protect your baby, it’s recommended that you receive the whooping cough vaccine between 20 and 32 weeks of each pregnancy, regardless of how recently you were last vaccinated. This will help boost your immunity and pass antibodies to your baby, providing them with protection in the first few months of life. Like the flu vaccine, this is also available for free under the NIP.
These vaccines not only safeguard your health but also provide critical protection for your baby during the early stages of life, helping reduce the risk of severe illness. It’s also a good idea to encourage family members and caregivers to stay up to date with their vaccinations, including flu and whooping cough, to create a safer environment for your newborn.
In conclusion, immunization during pregnancy is a simple yet powerful way to protect both you and your baby from preventable diseases. By staying informed and receiving recommended vaccines, such as the flu and whooping cough shots, you provide crucial early immunity for your newborn. Taking this step ensures a healthier pregnancy and gives your baby a stronger start in life.
Chemical Exposure During Pregnancy: Risks and Safety Precautions
During pregnancy, it’s essential to avoid exposure to certain harmful substances that can pose risks to you and your baby. These include second-hand tobacco smoke, household chemicals, radiation, bacteria and fungi, changes in atmospheric pressure (such as in certain work environments), and chemicals found in workplaces.
Chemicals that can harm your baby include certain antibiotics, sterilizing agents, strong cleaning supplies, lab materials, pesticides, and fertilizers. Exposure to these chemicals can occur through inhalation, ingestion, or skin contact, and the potential harm to your baby depends on the specific chemical and the level of exposure.
If your job involves handling or being around hazardous materials, it’s important to inform your employer. Legally, you have the right to request alternative duties to reduce exposure to harmful substances, and this protection applies to all pregnant employees, including casual workers. Additionally, it’s a good idea to carefully review product labels at home and choose pregnancy-safe cleaning supplies and personal care products to reduce unnecessary exposure. Always consult your healthcare provider before using any medications or chemicals during pregnancy to ensure safety.
Self-Care During Pregnancy: Prioritizing Your Health and Well-Being
Taking care of your mental health during pregnancy is just as crucial as managing your physical well-being. While it’s common to experience anxiety and stress during pregnancy, symptoms of antenatal anxiety or depression should not be ignored. Seeking help early is essential, as these conditions are treatable and there are effective strategies and resources available.
Prioritize rest and don’t hesitate to accept support from family and friends, especially if you have other children to care for. Incorporating relaxation techniques can also significantly alleviate stress and enhance your emotional well-being. Many women find that practices such as guided muscle relaxation, breathing exercises, and visualizing calm, peaceful scenes can be highly effective in managing anxiety. Additionally, engaging in regular physical activity, maintaining a balanced diet, and connecting with supportive communities or prenatal groups can further contribute to a positive mental state during pregnancy. If you’re struggling, remember that reaching out for professional support from a therapist or counselor can provide valuable assistance in navigating emotional challenges.