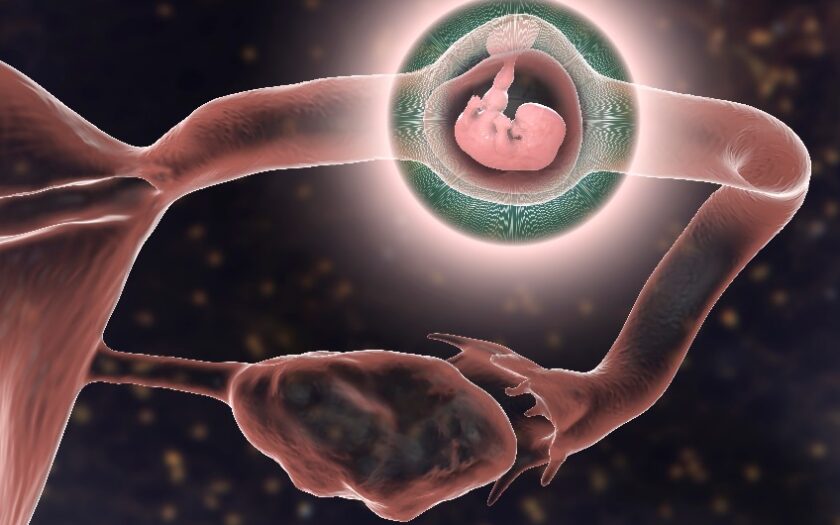
Ectopic pregnancy occurs when a fertilized egg implants outside the uterus, often in the fallopian tubes. This condition can pose serious risks and requires prompt medical attention to ensure the health and safety of the person affected. Understanding the symptoms and management options is crucial for timely diagnosis and treatment.
Recognizing and Treating Ectopic Pregnancy: A Complete Guide
An ectopic pregnancy occurs when a fertilized egg implants outside the uterus, most commonly in one of the fallopian tubes. This type of early pregnancy loss typically occurs 6-8 weeks after your last normal period. Although less common, ectopic pregnancies can also develop in the ovaries, cervix, other parts of the abdomen, or in a scar from a previous caesarean section.
Unfortunately, an ectopic pregnancy cannot result in a viable birth. It will either end in miscarriage or require medical intervention to terminate. If the ectopic pregnancy is located in a fallopian tube, it can lead to a rupture or tear, potentially causing severe internal bleeding. In such cases, it poses a significant risk to your health and can be life-threatening if not promptly treated.
Early Warning Signs of Ectopic Pregnancy: What to Look Out For
Ectopic pregnancy is a serious condition where a fertilized egg implants outside the uterus, often in a fallopian tube. Recognizing the early warning signs is crucial for prompt medical intervention, which can prevent serious complications. Understanding these symptoms can help ensure timely treatment and safeguard your health.
Ectopic pregnancies can present with a variety of signs and symptoms, including:
- vaginal bleeding or spotting. This may be light or heavy and can be mistaken for a normal period;
- abdominal (tummy) pain. Often one-sided, this pain can range from mild to severe and may come and go;
- back pain. Lower back pain can be persistent or intermittent;
- shoulder tip pain. Pain in the shoulder area, particularly on one side, can be a sign of internal bleeding and irritation of the diaphragm;
- nausea and vomiting. Persistent nausea and vomiting may accompany the abdominal pain;
- a fast heart rate. Increased heart rate can occur due to internal bleeding or shock.
- dizziness or faintness: These symptoms can result from blood loss or decreased blood pressure.
In addition to these symptoms, it’s crucial to be aware of sudden, severe abdominal pain, and signs of shock such as rapid breathing, pale skin, and confusion. If you experience any of these symptoms, seek immediate medical attention, as an ectopic pregnancy can be life-threatening if not promptly treated.
Early detection of an ectopic pregnancy is vital for minimizing risks and ensuring appropriate care. If you experience any of the warning signs, such as abnormal bleeding or severe pain, seek medical attention immediately. Prompt treatment can help prevent serious complications and protect your overall health.
Factors That Increase Your Risk of Ectopic Pregnancy
Understanding the factors that increase the risk of an ectopic pregnancy is crucial for early detection and management. Certain conditions and lifestyle choices can elevate the likelihood of an ectopic pregnancy, where the fertilised egg implants outside the uterus. By recognizing these risk factors, you can take proactive steps to safeguard your reproductive health and seek timely medical advice.
Ectopic pregnancies occur in approximately 1 in every 100 pregnancies. While many women with ectopic pregnancies may have no identifiable risk factors, certain conditions and factors can increase the likelihood of an ectopic pregnancy. These include:
- fertility Treatments. Procedures like in vitro fertilisation (IVF) can raise the risk;
- sexually Transmitted Infections (STIs). Past infections, such as chlamydia or gonorrhoea, can damage the fallopian tubes;
- damaged Fallopian Tubes. Scarring or blockages can prevent the fertilised egg from reaching the uterus;
- previous Abdominal Surgery. Past surgeries, including caesarean sections or operations for ovarian cysts, can increase risk;
- previous Tubal Sterilisation. Past sterilisation procedures can alter the normal function of the fallopian tubes;
- pregnancy While Using Contraceptives. An intrauterine device (IUD) or progestogen-only pill may not fully prevent pregnancy;
- smoking. Smoking is known to affect the fallopian tubes and overall reproductive health;
- age. Being 35 years old or older can increase the risk of an ectopic pregnancy due to changes in reproductive health.
Understanding these risk factors can help with early detection and management, but it’s important to note that having one or more of these factors does not guarantee an ectopic pregnancy. Regular prenatal care and monitoring can help ensure a healthy pregnancy.
Being aware of the factors that increase your risk of an ectopic pregnancy allows for better preparation and proactive management of your reproductive health. If you have any of these risk factors, it’s important to discuss them with your healthcare provider to monitor your pregnancy closely and address any potential issues early on. Taking these steps can help reduce complications and ensure you receive the appropriate care.
Diagnostic Approaches for Ectopic Pregnancy: What You Need to Know
Diagnosing an ectopic pregnancy involves a combination of clinical assessment and diagnostic tests to accurately identify the location of the pregnancy and determine the appropriate course of action. Early and precise diagnosis is crucial to manage the condition effectively and minimize risks to your health.
If your doctor suspects an ectopic pregnancy, they will start by asking detailed questions about your symptoms and medical history, including whether you are or could be pregnant.
To diagnose an ectopic pregnancy, your doctor will typically recommend several tests:
- blood Test. A blood test to measure levels of the pregnancy hormone human chorionic gonadotropin (hCG). Abnormal levels of hCG can indicate an ectopic pregnancy;
- ultrasound. An ultrasound scan, which may include a vaginal ultrasound, to visualize the location of the pregnancy. This helps in detecting whether the fertilized egg has implanted outside the uterus.
In some cases, additional diagnostic procedures like a laparoscopy might be needed if initial tests are inconclusive. Laparoscopy involves inserting a thin tube with a camera through a small incision in your abdomen to directly view the reproductive organs.
Early and accurate diagnosis of an ectopic pregnancy is essential for effective treatment and to reduce potential complications. By undergoing appropriate tests and evaluations, your healthcare provider can ensure timely intervention and better manage the condition. If you experience symptoms or have risk factors, consult your doctor promptly to safeguard your health and well-being.
Treatment Options for Ectopic Pregnancy: What You Need to Know
Your doctor will determine the appropriate treatment for an ectopic pregnancy based on its location, size, and your overall health. The treatment options may include medication, such as methotrexate, to stop the growth of the ectopic tissue, or surgery to remove the ectopic pregnancy and potentially repair any damaged tissues. In some cases, the approach may involve laparoscopic surgery for a less invasive procedure.
After your treatment, follow-up tests are crucial to ensure that the ectopic pregnancy has been fully resolved and that your hormone levels have returned to normal. This may include additional blood tests to monitor hormone levels and, if necessary, follow-up ultrasounds to confirm that there are no remaining ectopic tissues. Regular follow-ups help prevent complications and support your recovery.
How to Manage an Ectopic Pregnancy with a Watch-and-Wait Approach
If it appears that your ectopic pregnancy is resolving on its own, your doctor might suggest a “watch and wait” approach. This recommendation is typically made if you are feeling well or experiencing only mild discomfort, the ectopic pregnancy is small and has not ruptured, and your pregnancy hormone (hCG) levels are low and decreasing.
During this period, it’s essential to monitor your symptoms closely. Seek immediate medical attention by going to the nearest emergency department or calling emergency services (triple zero or 000) if you experience any of the following symptoms:
- severe abdominal pain;
- pain in your shoulder tip;
- heavy vaginal bleeding;
- dizziness or fainting.
Regular follow-up visits will be necessary to ensure that the ectopic pregnancy is resolving as expected and to manage any potential complications.
A watch-and-wait approach for managing an ectopic pregnancy can be effective under specific conditions, but it requires careful monitoring and prompt action if symptoms worsen. Regular follow-up with your healthcare provider is crucial to ensure the pregnancy is resolving and to address any potential complications quickly. Always seek immediate medical help if you experience severe symptoms to safeguard your health and well-being.
Medical Management of Ectopic Pregnancy: Options and Considerations
Medical management is a key option for treating ectopic pregnancy, particularly when the condition is diagnosed early and no complications are present. This approach typically involves the use of medication to stop the growth of the ectopic tissue, offering a non-surgical alternative. Understanding the criteria for medical management and potential outcomes is crucial for effective treatment and recovery.
Medication can be used to treat an ectopic pregnancy if:
- the ectopic pregnancy is very small;
- there are no signs of internal bleeding or rupture.
The medication commonly used is methotrexate, which is administered as an injection. Methotrexate works by stopping the growth of the ectopic tissue, but it may take some time to be effective. This treatment requires careful monitoring, and you may need follow-up appointments to ensure the medication is working and the ectopic tissue is resolving.
Methotrexate is not suitable for everyone. Some women might require additional doses of the medication or may need surgical intervention if the medication does not resolve the ectopic pregnancy or if complications arise. Your healthcare provider will determine the best course of action based on your specific situation.
Medical management of ectopic pregnancy can be an effective non-surgical option when the condition is detected early and the criteria are met. It involves careful monitoring and may require follow-up treatments to ensure the complete resolution of the ectopic tissue. For some patients, additional interventions such as surgery may be necessary, highlighting the importance of ongoing medical evaluation and personalized treatment plans.
Surgical Approaches for Ectopic Pregnancy: What You Need to Know
Surgery may be required to manage an ectopic pregnancy, particularly if there is internal bleeding or if the pregnancy poses a significant risk of bleeding. Surgery is also considered if medication is ineffective or unsuitable for your condition.
Typically, the surgery is performed using a minimally invasive technique called keyhole surgery (laparoscopy). This approach involves small incisions and is associated with quicker recovery times. However, in some cases, open surgery may be necessary, which involves a larger incision. If the ectopic pregnancy is located in a fallopian tube, it may need to be removed to ensure your health and safety.
Finding Support During and After an Ectopic Pregnancy: Resources and Guidance
An ectopic pregnancy is a type of early pregnancy loss, and it’s natural to experience grief and emotional distress. It’s important to seek support, and there are various resources available to help you through this difficult time. Speak with your doctor about accessing Medicare-funded counseling services with a psychologist, which they can arrange for you. Additionally, community support groups can offer comfort and guidance. For locating a psychologist, you can use the Healthdirect Service Finder tool to find one near you.
How an Ectopic Pregnancy May Affect Your Future Pregnancies
An ectopic pregnancy can impact your future fertility depending on various factors, such as the location of the ectopic pregnancy, the treatment used, and any underlying conditions. For example, if surgery was required to remove the ectopic pregnancy or a fallopian tube, this may affect your ability to conceive naturally. It is important to discuss your individual circumstances with your doctor, who can provide personalized information about how your fertility might be affected and suggest any necessary follow-up or fertility assessments.
Understanding the Risk: Chances of Experiencing Another Ectopic Pregnancy
If you’ve experienced an ectopic pregnancy, your risk of having another one in the future is increased. This heightened risk can be due to residual issues from the underlying causes that led to the first ectopic pregnancy, such as infections or anatomical abnormalities. Additionally, if your fallopian tube was damaged or scarred during the ectopic pregnancy, it may increase the likelihood of a future ectopic pregnancy.
It’s important to discuss your individual risk factors with your healthcare provider, who can offer personalized advice and management strategies for future pregnancies. Regular monitoring and early intervention can help address any issues promptly.
Guidelines for Resuming Sexual Activity After an Ectopic Pregnancy
After an ectopic pregnancy, it’s important to discuss with your doctor when it is safe to resume sexual activity. Your doctor can provide personalized advice based on your recovery and any specific considerations related to your health. Additionally, this is a good time to review your contraception options to prevent an unintended pregnancy and support your overall reproductive health.
Planning for Future Pregnancies: How Long to Wait After an Ectopic Pregnancy
If you’ve experienced an ectopic pregnancy, planning your next steps carefully is crucial. Knowing how long to wait before trying for another baby can help ensure your body is fully recovered and ready for a healthy pregnancy. Understanding the recommended waiting periods and following medical advice can contribute to a successful future pregnancy.
It’s generally advised to wait the following periods before trying to conceive again after an ectopic pregnancy:
- 2 months after surgery. This allows time for your body to heal and for any internal damage to recover;
- 3 to 4 months after taking medication (such as methotrexate). Methotrexate can linger in your system for a while and may pose risks to a new pregnancy. Ensuring it is completely cleared from your body is crucial for a healthy future pregnancy.
Once you become pregnant again, it’s important to notify your doctor as soon as possible. They will likely recommend an early pregnancy ultrasound to confirm that the pregnancy is developing normally in the uterus and not in another location, which helps in monitoring and managing your pregnancy effectively.
Planning for a future pregnancy after an ectopic pregnancy involves careful consideration and consultation with your healthcare provider. Adhering to the recommended waiting period allows your body to heal properly and reduces potential risks. By taking these steps, you can optimize your chances for a healthy and successful pregnancy in the future.